1. What is sexual desire ?
This is the mental and emotional interest in sexual activity — fantasies, urges, or the wish to be sexual desire with a partner or alone. In clinical practice the diagnostic categories shifted in recent years: desire and arousal are now commonly considered together when assessing women who have persistent reductions in interest and/or physical responsiveness that cause distress.
Why that matters: clinicians focus not only on frequency of sex but on whether the person feels bothered or impaired by the change.
2. How common is low desire in women?
Many women notice fluctuations in desire across life phases — pregnancy, postpartum, perimenopause/menopause, after major stress, or with illness. When these changes persist and cause emotional distress or relationship strain, they may meet criteria for a clinical diagnosis, and help is appropriate. (Prevalence estimates vary by age, culture and the measurement used.)
3. Common causes of low desire in women

Low desire in women most often reflects multiple overlapping factors — we call this a biopsychosocial problem. The main categories are:
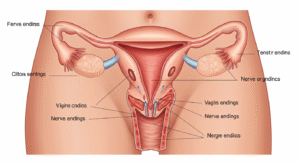
- Biological / medical: hormonal changes (pregnancy, breastfeeding, menopause), thyroid problems, diabetes, chronic pain, surgical changes, and some neurological conditions.
- Medications: many antidepressants and other drugs can lower libido — SSRIs are well-known for this side effect. If a medication change lines up with reduced desire, talk to your clinician rather than stopping medication abruptly.
- Psychological: depression, anxiety, past sexual trauma, body image, or low self-worth can reduce sexual interest.
- Relational: unresolved conflict, poor communication, mismatched desire levels, and trust issues often shrink desire.
- Lifestyle & sleep: chronic stress, poor sleep, excessive alcohol or substance use, and extreme fatigue make desire harder to access.
Because causes usually overlap, effective care looks beyond a single “fix.”
4. How clinicians assess low desire (what to expect)
A thorough assessment usually includes:
- A careful history of symptoms (how long, whether distressing, patterns).
- Review of medications and medical history.
- Targeted physical exam and (when indicated) lab tests — thyroid function, basic metabolic panel, hormone checks — guided by your history.
- Use of validated questionnaires like the Female Sexual Function Index (FSFI) to measure desire, arousal, pain and satisfaction. The FSFI is widely used in clinics and research as a screening and monitoring tool.
Diagnosis typically requires symptoms present for several months and causing personal distress; your clinician will rule out treatable medical causes before recommending specialized therapies.
5. Treatment options — practical and medical
The good news: many women improve with a tailored plan. Treatment commonly follows the biopsychosocial model.
a) Psychosocial treatments (first-line for many)
- Sex therapy and couples therapy: trained sex therapists help rebuild intimacy, repair communication, and use graded exercises to restore desire.
- Cognitive-behavioral and mindfulness-based therapies: useful when anxiety, negative thoughts or past trauma are contributors.
- Sensate focus and graded intimacy exercises: stepwise, non-demanding touch exercises that shift focus from performance to pleasure and safety.
International guidance supports a biopsychosocial treatment model and careful, individualized care.
b) Medical options and medications
- Hormonal treatments: For some women (especially with menopause-related changes) local vaginal estrogen or other hormone management can improve comfort and the sexual experience.
- Medications approved for HSDD in premenopausal women: Flibanserin (Addyi) and bremelanotide (Vyleesi) are FDA-approved options for acquired, generalized hypoactive sexual desire disorder in premenopausal women. These medicines have specific indications, benefits and side effects; they are not suitable for everyone and require clinical discussion before use.
- Testosterone therapy: Some guidelines and specialist societies offer narrow, closely monitored guidance for the off-label use of testosterone in selected women with HSDD; this requires careful hormonal testing and monitoring by a specialist.
Important safety note: medication choices should always be made with a clinician after reviewing your history, other drugs you take, and your health risks. Some options interact with alcohol or cause side effects like dizziness, nausea, or blood pressure changes.
6. At-home strategies you can try today
Small, consistent steps often matter more than one big intervention.
- Talk to your partner: try one short script — “I miss feeling close to you. Can we set aside 30 minutes this week just to talk, no phones, no interruptions?”
- Schedule non-sexual closeness: shared baths, walks, or lying together without pressure.
- Sleep and stress: set one boundary to improve sleep (lights out 30 minutes earlier, no screens).
- Mindful touch: 10–15 minutes of non-sexual, non-demanding touch (hands, shoulders) — shift attention to sensations, not performance.
- Check medications: if you suspect an antidepressant or other drug is affecting desire, don’t stop it — ask your prescriber about alternatives or dose adjustments.
- Pelvic floor physiotherapy: for women with pain or pelvic tension, a trained pelvic physiotherapist can make a big difference.
Start with one or two changes and track results rather than trying everything at once.
7. Helpful enhancements (worksheets, exercises, conversation starters)
- Weekly intimacy check-in sheet (5 minutes): what felt good this week? one request for next week? one worry?
- Sensate focus starter: set a 20-minute timer; spend 10 minutes exploring non-genital touch while focusing on breath; switch roles next session.
- Medication review checklist: list all prescriptions and over-the-counter drugs to bring to your appointment.
- Desire diary: note days you felt desire, context (sleep, mood, alcohol), and what was different — patterns emerge quickly.
These practical tools help translate clinical advice into day-to-day change.
8. When to see a specialist
Make an appointment if:
- Low sexual desire lasts months and causes distress.
- You or your partner feel the relationship is suffering.
- Pain or medical symptoms are present.
- You’re considering prescription therapies and want expert guidance.
If you’re in Hyderabad, Female Sexual Health by Dr. Kusuma offers confidential assessment and care at Androcare-Swetha Scans, 67-A, Journalist Colony, Road No 70, Jubilee Hills, Hyderabad-500033. Bookings and information: femalesexualhealth.in.
Author & review box
Author: Dr. Kusuma — Sexual Health Specialist with 10 years’ clinical experience.
Clinic: Female Sexual Health by Dr. Kusuma, Androcare-Swetha Scans, 67-A, Journalist Colony, Road No 70, Jubilee Hills, Hyderabad-500033. Website: femalesexualhealth.in.
Phone: 91 9000218377
Clinical review: Content reviewed by the Female Sexual Health multidisciplinary team for clinical accuracy and local applicability.