1. Why this article matters
Talking about sex problems can feel awkward. Yet these issues affect relationships, mental health and quality of life. If you’re reading this, you’ve already taken an important step — looking for clear, practical information. This guide explains causes, what a clinical assessment looks like, and the realistic sex treatment options available — in language you can use right away.
2. What we mean by “sex problem”
“Sex problems” is an umbrella term for difficulties that prevent you or your partner from enjoying sexual activity the way you want. Examples include decreased desire (low libido), difficulty with arousal, pain during sex, trouble reaching orgasm, anxiety around sex, and physical issues that affect comfort or function. Because this is broad, proper evaluation identifies the specific problem so the right sex treatment can be offered.
3. How common they are
Sex problems are very common. Studies show a significant proportion of women and men experience one or more sexual difficulties at some point in life. Frequency increases with life transitions (childbirth, menopause, chronic illness) and stress. The good news: many sex problem respond well to focused treatment once the cause is identified.
4. Common causes
Sex problems usually come from one or more overlapping areas:
Physical causes
- Hormonal changes (postpartum, perimenopause, menopause).
- Medical conditions (diabetes, thyroid disorders, cardiovascular disease).
- Medications (antidepressants, some blood pressure drugs).
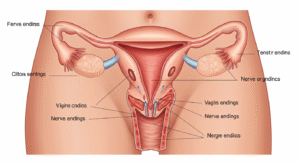
- Pelvic or genital conditions (endometriosis, vulvodynia, infections).
- Pain conditions (vaginismus, dyspareunia).
Psychological causes
- Stress, anxiety, depression.
- Past sexual trauma (requires trauma-informed care).
- Body image concerns.
- Performance anxiety.
Relational and social causes
- Communication breakdown with partner.
- Mismatched desire levels.
- Life stressors (work, childcare, finances).
Because causes overlap, a combined approach often works best.

5. How clinicians evaluate sex problems (what to expect)
A clinic visit usually includes:
- History: Medical, sexual, relationship, medication and mental health review.
- Symptom review: Timing, pattern, triggers, and what makes issues better/worse.
- Physical exam: Pelvic exam or general exam if indicated; sometimes simple tests (blood tests for hormones, thyroid, blood sugar).
- Questionnaires: Validated forms to quantify symptoms and guide treatment.
- Collaborative plan: A clear, stepwise sex treatment plan tailored to you.
Expect a respectful, non-judgmental conversation. If you’re nervous, bring notes or have a partner join if you both agree.
6. Practical sex treatment options
Sex treatment is rarely one-size-fits-all. Here are common, evidence-based options:
Medical treatments
- Hormonal therapy: Topical estrogen (for vaginal dryness), systemic hormone therapy when appropriate.
- Medication review & changes: If an antidepressant or other drug contributes, we may adjust dose or switch medications with your doctor.
- Topical treatments and lubricants: Water-based or silicone lubricants and prescribed topical agents for dryness or vulvar atrophy.
- Pelvic pain interventions: Local treatments, nerve blocks (in specialist centers), or topical anaesthetics as appropriate.
Psychosexual therapy & counselling
- Cognitive-behavioral therapy (CBT): For anxiety or negative beliefs about sex.
- Sex therapy: Practical exercises, sensate focus, and communication coaching for couples.
- Trauma-informed therapy: For patients with a history of sexual trauma.
Pelvic health rehab
- Pelvic floor physiotherapy: Effective for pain, vaginismus, or muscle dysfunction.
- Biofeedback and relaxation training.
Devices and assistive options
- Vaginal dilators (graded therapy for vaginismus).
- Vibratory therapy for some types of arousal or orgasm difficulty (used under guidance).
- Pelvic floor stimulators when indicated.
Lifestyle & complementary
- Sleep, exercise, nutrition — poor sleep or high stress reduces libido.
- Mindfulness and paced breathing — reduce performance anxiety.
- Couple communication exercises — regular check-ins about intimacy.
(Use of the relevant keyword: Sex treatment — included naturally.)
Most effective plans mix medical and psychological strategies and involve the partner when helpful.
7. Self-care and partner strategies you can start today
- Start a “positive intimacy” diary: note non-sexual affectionate moments to rebuild connection.
- Schedule brief, pressure-free time together: intimacy doesn’t need to be sexual to count.
- Try a lubrication-first approach: apply lubricant liberally for comfort and reduced pain.
- Mindfulness practice (5–10 min/day): reduces anxiety and improves body awareness.
- Open one sentence conversation with partner: “I want to talk about our sex life — can we set 15 minutes this week?” Use non-blaming language and focus on feelings and needs.
8. Red flags — when to seek urgent help
Seek prompt care if you have:
- Sudden, severe pelvic pain.
- Unexplained vaginal bleeding, fever, or symptoms of infection.
- Pain so intense it causes fainting or inability to function.
If you’re in immediate distress (physical or emotional) call local emergency services.
9. Helpful enhancements
Printable checklist — “Before your appointment”
- List of symptoms and when they started.
- Current medications & supplements.
- Recent relevant medical history (surgeries, childbirth).
- One or two goals for treatment (e.g., “reduce pain” or “increase desire”).
- Any questions you want answered.
Conversation starter script
- “I’ve been noticing [brief symptom], and it’s worrying me. Can we talk about it and see what help we can get?”
Clinic-based resources
- Pelvic physiotherapy referrals.
- Psychosexual counselling contacts.
- Patient information leaflets on topical estrogen and lubricants.
10.FAQ
Q: Are sex problems normal?
Q: How long does sex treatment take to work?
Q: Will my partner need to be involved?
Q: Are there simple tests for sexual problems?
Q: Is sex therapy different from counselling?
Q: Can medication fix low libido?
Q: Is pelvic physiotherapy painful?
Q: What should I bring to my first appointment?
Final notes
If “sex problems” are affecting your life, remember: help exists and asking for it is the smart move. Start with a confidential consultation where your concerns are heard and a clear plan is created. For residents of Hyderabad, Female Sexual Health by Dr. Kusuma offers targeted evaluations and integrated sex treatment plans — visit femalesexualhealth.in or come by Androcare-Swetha scans, 67-A Journalist colony, Road no 70, Jubilee hills, Hyderabad-500033 or Phone: 91 9000218377 to book a confidential appointment.
Author & review box — Female Sexual Health by Dr. Kusuma
Author: Dr. Kusuma — Founder, Female Sexual Health. Clinician with 10 years’ experience helping women and couples manage sexual difficulties with individualized, respectful care.
Clinic: Female Sexual Health by Dr. Kusuma
Location: Androcare-Swetha scans, 67-A, Journalist colony, Road no 70, Jubilee hills, Hyderabad-500033
Website: femalesexualhealth.in
What we offer: Comprehensive evaluation, individualized sex treatment plans, pelvic physiotherapy referrals, psychosexual therapy coordination, and follow-up care tailored to busy lives.