1 — Quick overview: what we mean by female sexual problems
“Female sexual problems” refers to difficulties with desire, arousal, orgasm or pain during sex (for example, hypoactive sexual desire disorder, arousal disorder, orgasmic disorder, and dyspareunia). These can have medical, hormonal, medication-related, psychological, relationship or pelvic-floor causes — often more than one at the same time. Because of that complexity, medicines are rarely the only answer.
(For clarity: the phrase Medicine for female sex problems appears through this article to help you find this content in search results.)
2 — How medicines fit into treatment
Medicines are most useful when there is a clear biological or hormonal contributor (for example, menopausal vaginal atrophy causing pain, or a neurotransmitter-related desire disorder). Even then, the best outcomes come from combining medication with counseling, partner communication work and pelvic physical therapy when needed. Evidence and official guidance emphasize a combined approach rather than medication alone.
3 — Medicines that are approved and commonly used
Below are medicines with stronger regulatory or evidence backing. I’ll note what they treat and any important safety points.
- Flibanserin (brand: Addyi) — approved for acquired, generalized hypoactive sexual desire disorder (HSDD) in premenopausal women. It’s a daily pill that works on brain neurotransmitters (serotonin/dopamine). Common side effects include dizziness, sleepiness and low blood pressure—interactions (especially with alcohol and some medicines) are important.
- Bremelanotide (brand: Vyleesi) — an on-demand injectable approved for HSDD in premenopausal women. It’s used before anticipated sexual activity and acts at melanocortin receptors. Some patients report nausea or increased blood pressure.
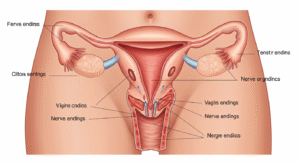
- Ospemifene (brand: Osphena) — an oral selective estrogen receptor modulator (SERM) approved to treat moderate-to-severe dyspareunia (pain with sex) due to menopausal vaginal atrophy. It’s aimed at improving vaginal tissues and reducing pain. Standard precautions for estrogenic drugs apply.
- Intravaginal prasterone (brand: Intrarosa) — a vaginal insert (DHEA/prasterone) approved for postmenopausal dyspareunia. It acts locally to improve vaginal tissue quality and reduce pain.
- Topical vaginal estrogen (gels, creams, rings) — frequently recommended for genitourinary syndrome of menopause (thinning, dryness, pain). They act locally with less systemic exposure than oral estrogens and are very effective for vaginal dryness and pain.
4 — Medicines with limited or mixed evidence
Testosterone therapy (often topical or transdermal) may help low sexual desire in some postmenopausal women, but it’s generally used off-label and requires specialist oversight and monitoring for side effects. Major society guidance urges caution and careful risk–benefit discussion. (Lippincott Journals)
PDE5 inhibitors (e.g., sildenafil) — effective in men but evidence in women is mixed. Some studies show benefit for specific situations (for example, erectile-function–affecting partner medication effects, or arousal problems tied to vascular response), but results are inconsistent and not routinely recommended as a first-line sex medicine for most women.
Many other “off-label” approaches have small studies but not consistent benefit; that’s why a tailored plan from a specialist matters.

5 — Non-drug treatments that matter
- Sex therapy / cognitive behavioral therapy: Proven to help desire, arousal and pain-related issues when psychological or relational factors are present.
- Pelvic floor physical therapy: Essential for pain, vaginismus, or muscle-related pain with sex.
- Vaginal lubricants and long-acting moisturizers: Over-the-counter but high impact for dryness and pain.
- Medication review: SSRIs, antihypertensives and other drugs can reduce desire or cause sexual side effects — changing meds can help.
- Lifestyle adjustments: Sleep, stress management, alcohol moderation and managing chronic illness (diabetes, thyroid issues) improve outcomes.
6 — How we decide what’s best
When I assess patients in clinic I follow a consistent approach. Here’s a short checklist you can use before your appointment:
- Medical history (meds, mental health, surgeries, childbirth, chronic disease)
- Sexual history (onset, context, distress level, partner issues)
- Symptom mapping (desire vs arousal vs orgasm vs pain)
- Physical exam (including pelvic exam when appropriate)
- Targeted labs (thyroid, HbA1c, hormones—only when indicated)
- Review of previous treatments and their effects
- Create a combined plan: medicine (if indicated) + therapy + pelvic care
This is how we reduce guesswork and pick a safe, evidence-based sex medicine or combination plan.
7 — Helpful enhancements for patients
- Pre-visit checklist (bring list of meds, note when problem started, what makes it worse/better).
- Communication scripts to discuss sexual concerns with your partner (short, neutral, specific).
- Symptom diary for 4 weeks — note desire, episodes of intimacy, pain, mood and medications.
- When starting a medicine: track side effects and response for 8–12 weeks unless the drug label says otherwise.
8 — Where to get help: Female Sexual Health by Dr Kusuma
If you’re in Hyderabad and would prefer an in-person specialist, Female Sexual Health by Dr Kusuma sees patients at:
Androcare-Swetha Scans
67-A, Journalist Colony, Road No. 70, Jubilee Hills, Hyderabad — 500033
Website: femalesexualhealth.in
At our clinic we combine medical assessment, targeted medicines where appropriate, pelvic physiotherapy referrals, and sex therapy or couples counseling options. If you think a medicine for female sex problems might help you, schedule a detailed consult so we can tailor the plan safely.
9 — Safety first: important cautions
- Don’t start prescription medications for sexual problems without a medical evaluation. Some medicines interact with alcohol, other drugs, or have cardiovascular or liver risks.
- If you have uncontrolled high blood pressure, heart disease, or are pregnant, many sex medicines are inappropriate.
- Discuss fertility goals before starting hormonal or systemic medicines.
FAQ
Q: Are there pills that fix low sexual desire in women?
A: There are two FDA-approved options for premenopausal hypoactive sexual desire disorder — flibanserin (daily pill) and bremelanotide (on-demand injection). They can help some women but are not a cure-all and have side effects and interaction considerations. Discuss risks and likely benefits with a specialist.
Q: What if sex is painful after menopause?
A: Local vaginal estrogen, ospemifene (oral SERM) or intravaginal prasterone can improve vaginal tissues and reduce pain. Over-the-counter lubricants and moisturizers help too.
Q: Can erectile-dysfunction drugs like Viagra help?
A: Evidence is mixed. Some women benefit in specific situations, but these drugs aren’t a routine first-line therapy for most female sexual problems.
Q: Is testosterone safe for women?
A: In select cases (often postmenopausal), low-dose testosterone can help desire, but it’s usually off-label and requires specialist monitoring. Society guidelines call for careful discussion of risks and close follow-up.
Q: How long before I see benefit from a sex medicine?
A: Depends on the drug: some (like bremelanotide) are used on-demand; others (like flibanserin) need weeks of daily dosing. For tissue-targeting treatments (vaginal estrogen/prasterone) expect gradual improvement over several weeks. Your clinician will set expectations based on the chosen medicine.
Q: How do I start?
A: Make an appointment for a specialist consultation (bring a list of medications and a brief symptom history). If you’re in Hyderabad, visit Female Sexual Health by Dr Kusuma at Androcare-Swetha Scans or book via femalesexualhealth.in.