The Role of Sex Medicine in Women's Sexual Health: A Comprehensive Guide

For many women, sexual health is a private and often unspoken topic. Yet, a fulfilling sexual life is a vital component of overall well-being and quality of life. When issues arise, such as low libido, difficulty with arousal, or painful intercourse, it can significantly impact relationships, self-esteem, and happiness. Fortunately, advancements in medical science have led to various forms of sex medicine specifically designed to address these complex challenges in women. This comprehensive guide aims to shed light on how sex medicine is transforming women’s sexual health, offering hope and solutions.
Understanding Women’s Sexual Health Challenges
Female sexual dysfunction (FSD) is a broad term encompassing various issues that prevent a woman from experiencing satisfaction during sexual activity. These issues can stem from a complex interplay of physical, psychological, hormonal, and relationship factors. Understanding these challenges is the first step toward finding effective solutions.
Common Conditions Affecting Female Sexual Function
- Hypoactive Sexual Desire Disorder (HSDD): Characterized by a persistent or recurrent deficiency (or absence) of sexual fantasies and desire for sexual activity.
- Female Arousal Disorder: Difficulty achieving or maintaining sufficient sexual arousal, leading to distress.
- Female Orgasmic Disorder: Difficulty, delay, or absence of orgasm following sufficient sexual stimulation.
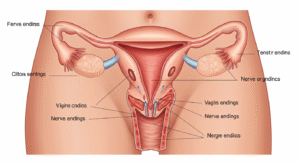
- Genito-Pelvic Pain/Penetration Disorder (GPPD): Persistent or recurrent difficulties with vaginal penetration, marked by pain, anxiety, or pelvic floor muscle tension.
- Vaginal Dryness: Often linked to menopause, leading to discomfort or pain during intercourse.
What is Sex Medicine for Women?
Sex medicine for women refers to a range of pharmaceutical treatments, hormonal therapies, and other medical interventions designed to alleviate symptoms of female sexual dysfunction. Unlike a one-size-fits-all approach, these medicines are tailored to address specific underlying causes, helping women regain comfort, desire, and satisfaction.
How Sex Medicine Addresses Female Sexual Dysfunction (FSD)
These medications work through various mechanisms. Some target neurotransmitters in the brain to boost desire, while others address hormonal imbalances or improve blood flow to genital areas. The goal is always to improve the physiological and psychological components necessary for a healthy sexual response, alleviating distress and improving sexual quality of life.
Types of Sex Medicine for Women
The landscape of sex medicine for women is evolving, offering several approaches depending on the diagnosis.
Prescription Medications
- Flibanserin (Addyi): Approved for premenopausal women with HSDD. It works on neurotransmitters in the brain, like serotonin and dopamine, to help balance chemicals related to sexual desire.
- Bremelanotide (Vyleesi): Also for premenopausal women with HSDD, this injection works on melanocortin receptors in the brain to increase sexual desire.
Hormonal Therapies
- Estrogen Therapy: Often prescribed for postmenopausal women experiencing vaginal dryness, pain during intercourse (dyspareunia), and thinning of vaginal tissues (atrophy). Available in oral, patch, cream, or ring forms. Localized estrogen therapy specifically targets vaginal symptoms with minimal systemic absorption.
- Testosterone Therapy: While not FDA-approved for FSD, some healthcare providers may prescribe low-dose testosterone off-label for women with persistent low libido, particularly after menopause or oophorectomy, under careful monitoring.
Non-Hormonal Options
- Ospemifene (Osphena): An oral medication for postmenopausal women experiencing moderate to severe dyspareunia (painful intercourse) due to vaginal atrophy. It acts like estrogen on vaginal tissue without affecting breast or uterine tissue in the same way.
- Prasterone (Intrarosa): A vaginal insert containing DHEA, a steroid that converts into estrogens and androgens within vaginal cells to improve symptoms of dyspareunia due to menopause.
Emerging Therapies and Natural Approaches
Research continues into new treatments, including localized creams, gels, and devices. Additionally, many women explore natural supplements and lifestyle changes, though their efficacy can vary and should always be discussed with a doctor. These are often considered complementary rather than standalone sex medicine.
The Benefits and Considerations of Sex Medicine
Deciding whether to use sex medicine is a personal choice that requires careful consideration of potential benefits against possible risks and side effects.
Potential Advantages
- Improved sexual desire and arousal.
- Reduction in pain during intercourse.
- Enhanced orgasm potential.
- Greater sexual satisfaction and overall quality of life.
- Improved body image and self-esteem.
- Stronger intimate relationships.
Important Side Effects and Safety Profile
Like all medications, sex medicines for women come with potential side effects. These can range from nausea, dizziness, and fatigue (with Flibanserin) to injection site reactions (with Bremelanotide) or local irritation (with vaginal therapies). Hormonal therapies carry their own set of considerations, including risks of blood clots or certain cancers in specific patient populations. It is paramount to have a thorough discussion with a healthcare provider to assess your individual health profile and determine the safest and most effective treatment plan.
Finding the Right Sex Medicine: Consulting a Healthcare Professional
Navigating the options for women’s sexual health can be overwhelming. This is where professional medical guidance becomes indispensable. A doctor can accurately diagnose the underlying cause of sexual dysfunction, rule out other medical conditions, and recommend the most appropriate sex medicine or combination of therapies.
Personalized Treatment Plans
Your healthcare provider will consider your medical history, current medications, lifestyle, and specific sexual concerns to create a personalized treatment plan. This may involve not only medication but also lifestyle adjustments, counseling, or other therapies. Don’t hesitate to seek expert advice; your well-being is worth it. For a comprehensive consultation on your sexual health, consider visiting our medical treatment services page.
Beyond Medication: Holistic Approaches to Women’s Sexual Wellness
While sex medicine offers targeted solutions, it’s often most effective when integrated into a broader approach to sexual wellness. This can include:
- Psychosexual Counseling: Addressing psychological factors like anxiety, stress, body image, or relationship issues.
- Lifestyle Changes: Regular exercise, a balanced diet, stress reduction, and adequate sleep can all positively impact sexual health.
- Pelvic Floor Physical Therapy: Beneficial for addressing pain or muscle tension related to sexual activity.
- Communication: Open and honest communication with a partner is crucial for a healthy sexual relationship.
Empowering Your Sexual Health Journey
The journey to improved sexual health is deeply personal. With the right information, professional guidance, and a willingness to explore available options, women can overcome sexual challenges and reclaim a fulfilling intimate life. Sex medicine is a powerful tool in this journey, offering specific solutions where they are needed most.
Ready to take the next step towards understanding and improving your sexual health? Contact us today for a confidential consultation.
Frequently Asked Questions (FAQ)
Q1: Is there a “female Viagra”?
A1: While there isn’t an exact “female Viagra” that works by increasing blood flow to the genitals in the same way as male Viagra, medications like Flibanserin (Addyi) and Bremelanotide (Vyleesi) are sometimes referred to as such because they address female sexual desire issues. They work on brain chemistry rather than blood flow.
Q2: How effective are sex medicines for low libido in women?
A2: The effectiveness of sex medicines like Flibanserin and Bremelanotide for low libido (HSDD) varies among individuals. Clinical trials showed modest but statistically significant improvements in sexual desire and satisfying sexual events for some women. Success often depends on accurately identifying the underlying cause of low libido and a personalized approach.
Q3: Are there natural alternatives to sex medicine for women?
A3: Many women explore natural alternatives, including herbal supplements (e.g., Maca, Ginseng), dietary changes, exercise, and stress reduction techniques. While some individuals report benefits, scientific evidence supporting their efficacy for FSD is often limited compared to prescription medications. Always consult a healthcare provider before trying natural supplements, especially if you are on other medications.
Q4: What are the side effects of female sex medicine?
A4: Side effects vary depending on the specific medication. For Flibanserin, common side effects include dizziness, nausea, fatigue, and low blood pressure, especially when consumed with alcohol. Bremelanotide can cause nausea, flushing, and injection site reactions. Hormonal therapies have their own potential side effects and risks, which your doctor will discuss thoroughly.
Q5: How do I know if sex medicine is right for me?
A5: The best way to determine if sex medicine is right for you is through a comprehensive consultation with a healthcare professional, such as a gynecologist or a sexual health specialist. They can evaluate your symptoms, medical history, and lifestyle to diagnose any underlying conditions and recommend the most appropriate and safest treatment options tailored to your needs.
Patient Testimonial
“I had been struggling with low desire for years, feeling isolated and frustrated. After speaking with a specialist and exploring options, including sex medicine, I’ve seen a remarkable improvement. It wasn’t just the medication; it was the comprehensive support that helped me rediscover intimacy and confidence. I feel like myself again!”
— Satisfied Patient, A.R.